








Tuberculosis
Adam Guttentag M.D.
10/03









History
•“White plague”, “Consumption”
•Tuberculous changes in mummy spines
•460 BC - Hippocrates describes “phthisis” as most commondeadly disease.
•1720 - infectious nature of disease described
•1859 - sanatorium therapy
•1882 - tubercle bacillus identified by Koch
•1894 - artificial ptx- earliest plombage therapy









History
–At the beginning of the 20th century
•Leading cause of death of adults in US
•1 of 7 deaths in US and Europe
–1921 - BCG vaccine introduced
•Attenuated form of M. bovis
•Antibiotics
–1944 - streptomycin
–1949 - p-amino salicylic acid
–1952 - isoniazid
–1962 - ethambutol
–1963 - rifampin










TB therapy c. 1940









Tuberculosis Worldwide
•2 billion people infected
•2 million deaths / year
•95% of cases in developing countries
•Highest incidence in Asia (40% of cases)
–SE Asia: 237/100K
–Subsaharan Africa: 191/100K
–US: 5.2/100K (2002)
•Incidence increasing in eastern Europe and Africa
•HIV, MDR TB worsening problems
–MDR incidence 48% in Nepal










Tuberculosis 2002
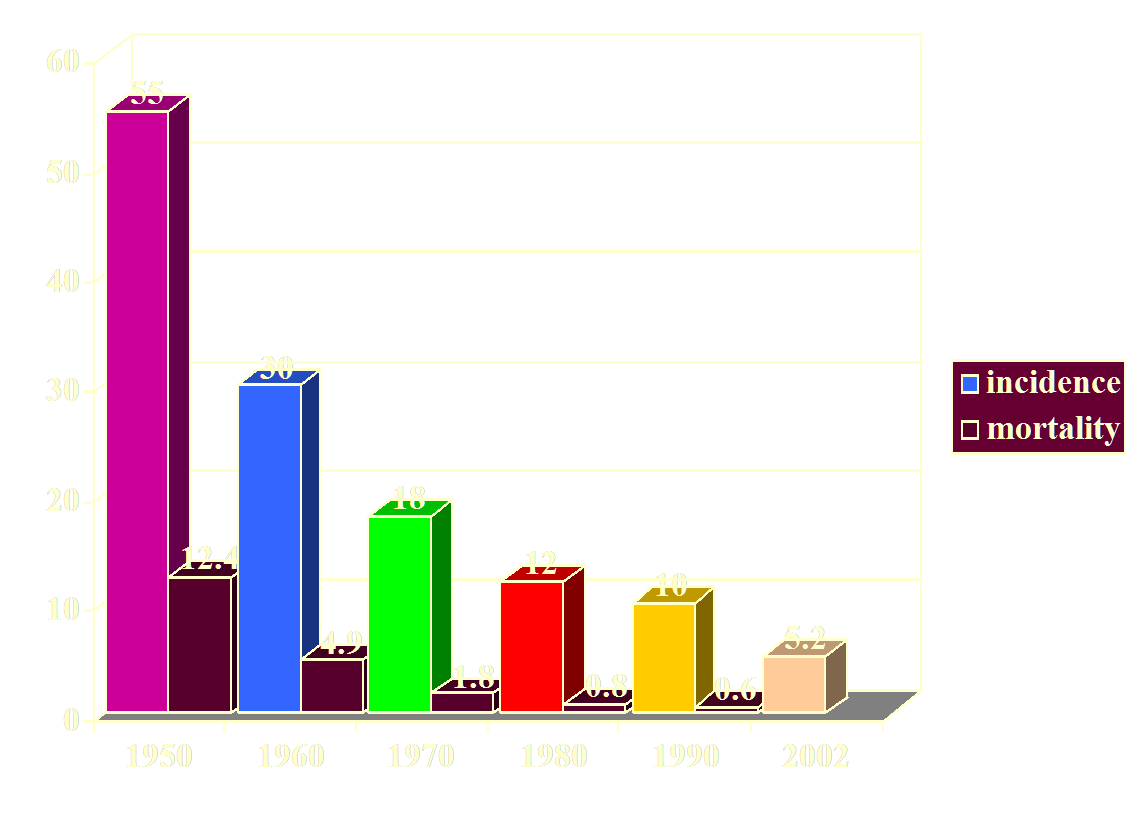
Incidence in US per 100,000 population









Tuberculosis 2002
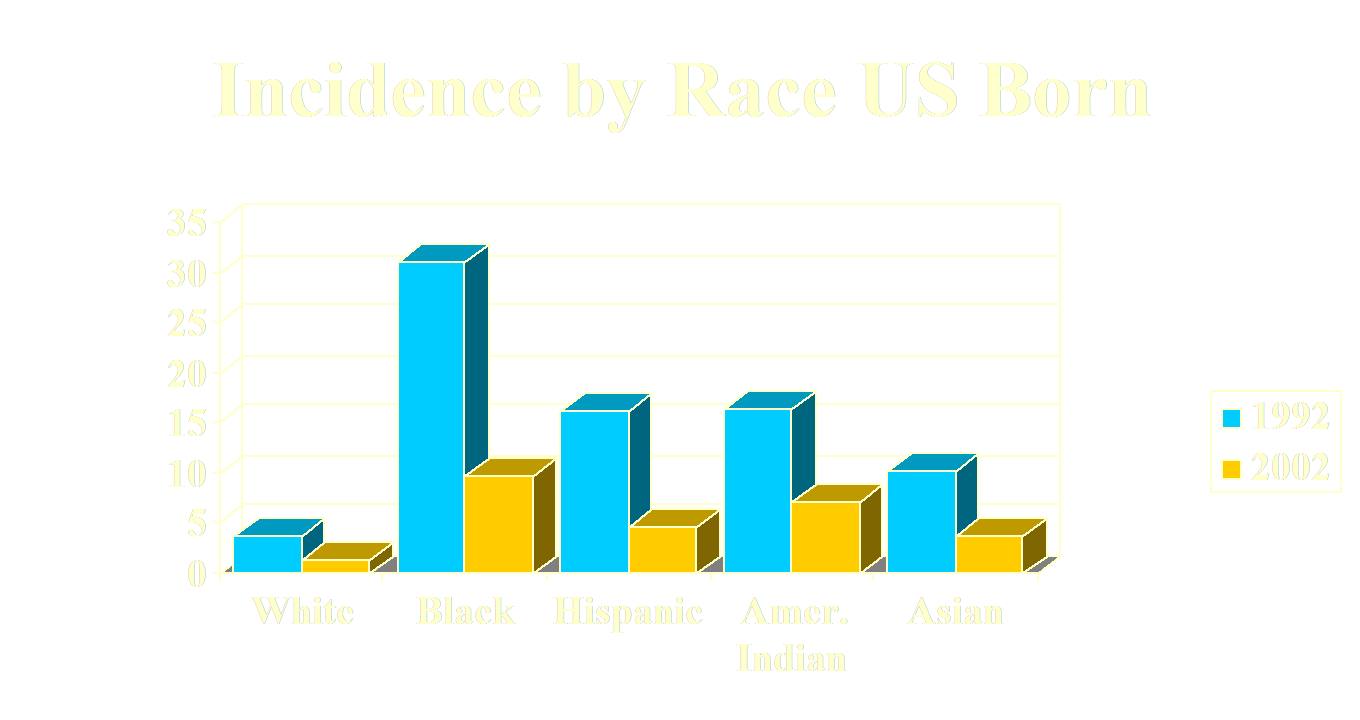
Significant decline among all racial groups









Tuberculosis in PA
•Overall rate 2.8/100K, 1/2 of US rate
–Philadelphia 9.5/100K (41% of PA cases)
–44% foreign born, similar to US rate
–9.4% INH resistant
–2.3% multidrug resistant
–Racial rates similar to US except:
•Asians 37.2/100K
•AEMC ~10 cases/year









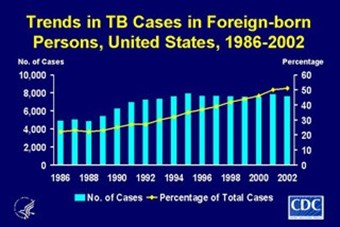
TB in Foreign Born Americans
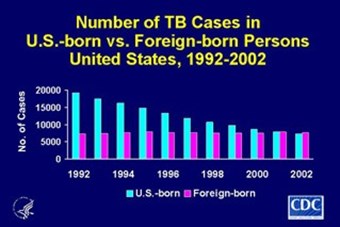










Tuberculosis 2002
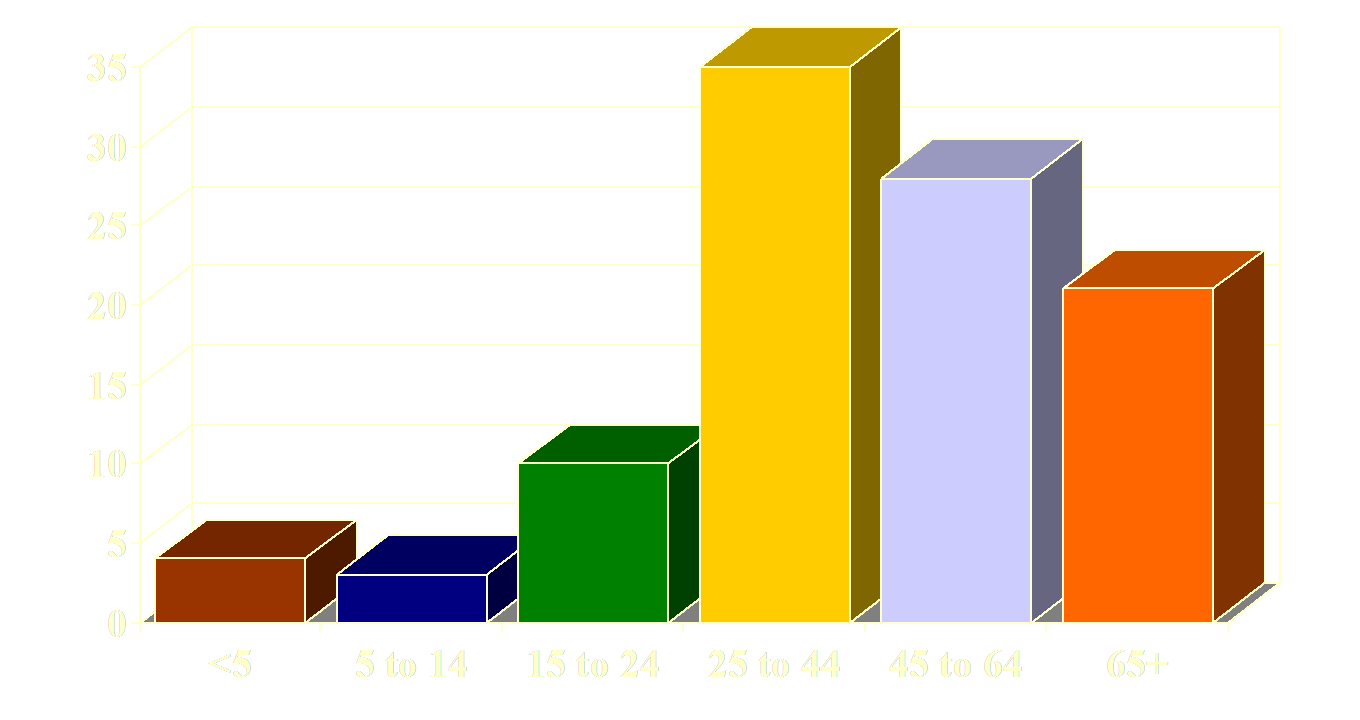










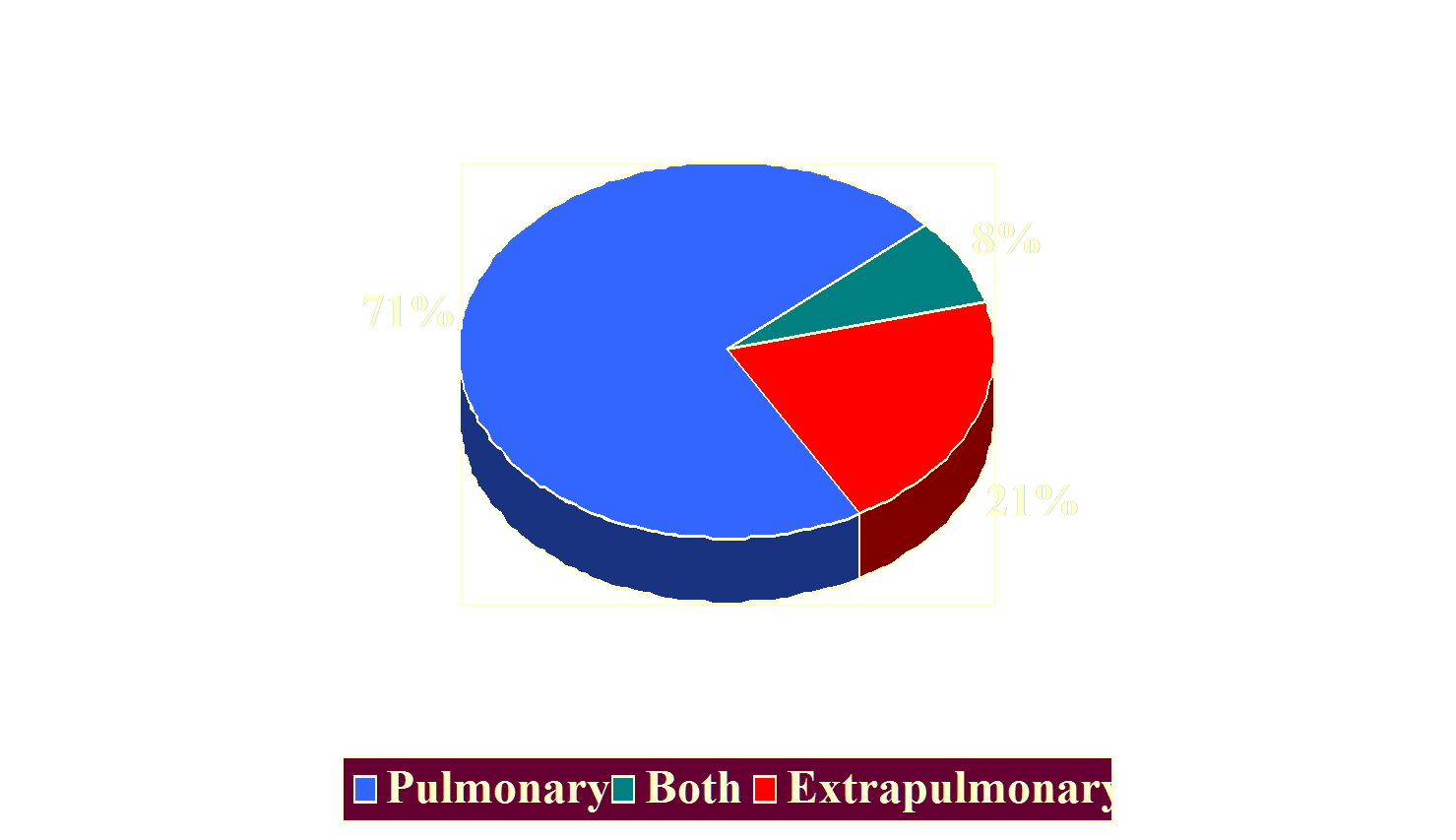
Tuberculosis 2002Sites of Disease









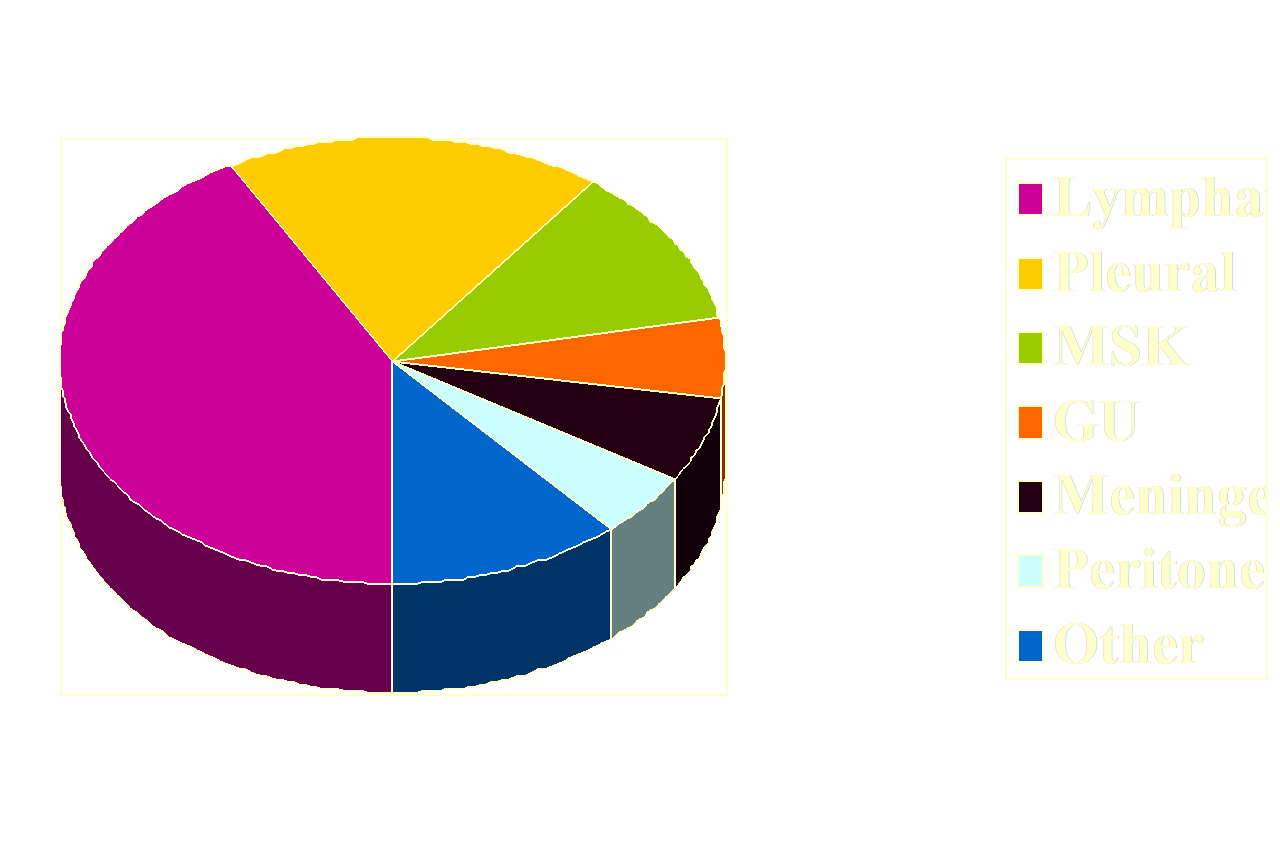
Tuberculosis 2002Extra-pulmonary Locations









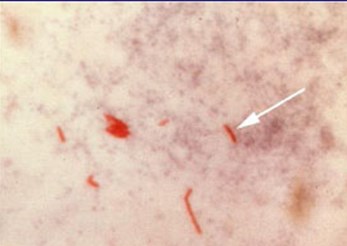
Mycobacterium tuberculosis
•Obligate aerobe
•Thick waxy lipid cell wall
–High resistance to drying, acid, alkali.
–Remains alive for long periods outside or intracellular.
•Retains carbol- fuschin stain on acid wash (acidfast)
–Also other mycobacteria, Nocardia, Rhodococcus,Corynebacterium sp.









Infection
•Droplet nuclei (1-5 microns)
–May be suspended in air for hours.
•Transmission of infection to 21-23% of closecontacts.
•Transmission to a close contact depends on:
–Duration of exposure
–Local environment
•Ventilation
•Crowding
–Number of organisms expelled into air
–Virulence of organisms









Infection
•Larger droplets deposited on airway mucosa,expectorated or swallowed.
•Smaller droplets deposited in alveoli
–Infection develops in lung, and in regional lymphnodes.
–Systemic dissemination of bacilli.
•Delayed immune response (2-10 weeks)
–Cell mediated immunity - mkills bacillus
–Delayed hypersensitivity - necrotizing granuloma
–PPD conversion
–Confers resistance to later infection.









Alveolar
M
Virulence andgeneticsusceptibilityvs. bactericidalactivity of m
Droplet inhaled into alveolus
Pathogenesis
Granulomaformation,Latent infection
CellMediatedImmunity
Regional lymphnodes and beyond









Pulmonary Tuberculosis
•Primary Infection
•Progressive Primary TB
•Latent TB Infection
•Postprimary TB
•Miliary TB









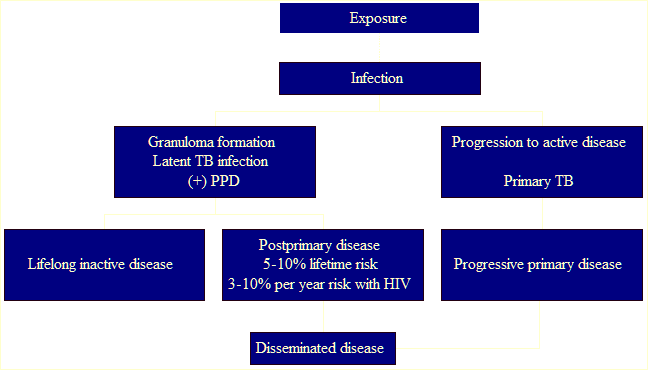
95%
5%
30%









Primary TuberculosisClinical Sx
•Children:
–Primary infection usually Asx or unrecognized
–Of young PPD converters:
•~40% had nonspecific fever, cough
•>90% clinically well
•75% with normal CXR
•<10% develop clinically apparent TB









Primary TuberculosisClinical Sx
•Adults
–>80% with clinical sx at primary infection
•Fever (40%)
•Cough
•Weight loss
•Hemoptysis
–Children and elderly likely to have atypicalpresentation









Primary InfectionRadiology
•Lymphadenopathy
–Prevalence decreases with age.
•100% in young children.
•10% in older adults.
–Right paratracheal most common.
–Low attenuation center of large LN’s.
–May be only abnormality in children (1/3).
–Rare to have no adenopathy in children .
–Common in severe HIV disease (CD4 <200/mm3).









Primary InfectionRadiology
•Parenchymal disease
–Usually consolidation
•Segmental or lobar
•Right side most common, based on granulomalocation
•Airway obstruction causing atelectasis or airtrapping more common in children
–Smaller airways, less stiff cartilage, more LAD.
–Delayed hypersensitivity response causescaseous necrosis and granuloma formation.



















Primary Infection
•Healing of primary focus
–Ghon focus in lung
–Ranke complex - calcifiedlung focus and hilar ormediastinal LN
–Dystrophic Ca++ may formin caseous material
–Surrounded by fibrosis










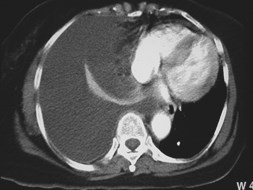
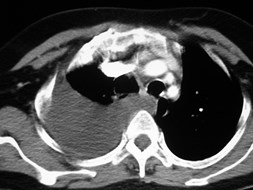
Pleural Effusion
•More common in primary infection
–Seen 3-6 months following exposure.
–29-38% of adults, uncommon in children.
–Typically unilateral on side of 10 infection.
–Only sign of disease in 5%.
–May precede appearance of parenchymal lung disease.
•Less common in postprimary disease
•Pleural fluid culture (+) in 20-40%
•Closed pleural Bx (+) in 65-75%
•True empyema--smears and cx usually positive
•Empyema necessitans











































Progressive Primary TB
•Disease not contained by delayed immunity.
•Progressive parenchymal destruction at siteof initial infection.
•Appearance similar to postprimary disease.









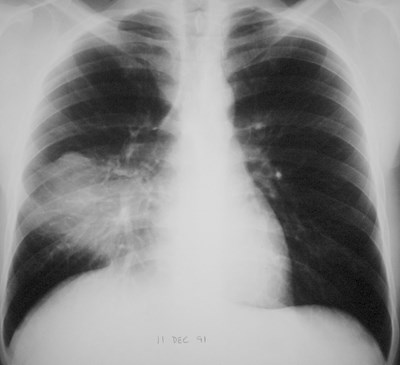
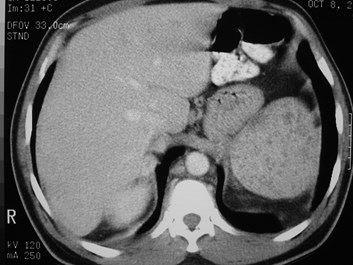
AIDS Patient




















Latent TB Infection
•+ PPD
•Patient asymptomatic
•No progressive inflammation and tissue necrosis
•Organisms inside caseating granulomas
•Organisms remain viable for many years










Postprimary (Reactivation) TB
•Active infection months to yearsafter initial infection.
•Formerly great majority of adultcases:
–In past, most were infected as children,reactivated as adults.
–Now, only about 60% of adult cases inUS.









Postprimary (Reactivation) TB
Risk factors forreactivation:
•HIV•HIV
•Diabetes
•Recent infection
•Steroids and otherimmunosupressives
•Silicosis
•Hematologic malignancy
•ESRD
•Low body weight









Postprimary (Reactivation) TB
•Can occur in any organ, most common in lungs.
•Upper lobes (apical and posterior segments) in85%.
•Superior segments of lower lobes in 12%.
–Higher O2 tension.
–Less lymphatic drainage.









Postprimary (Reactivation) TBProgression
PO2 locally acidic caseous material
# of organisms
Organisms enterbronchial tree
Spread to other parts oflungs and bronchial tree
Infectivity
Active infection
Cavity formation









Postprimary (Reactivation) TB
•Once infection becomes active again:
–Form of disease depends on host response vsvirulence of organism.
–Outcomes:
•Cavity formation with spread of infection
–Progressive destruction of lung tissue
–“galloping consumption”
•Tuberculoma formation
–Masslike infection without cavitation
•Healing with fibrosis and calcification









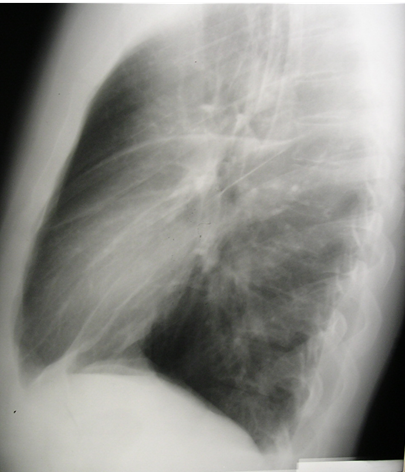
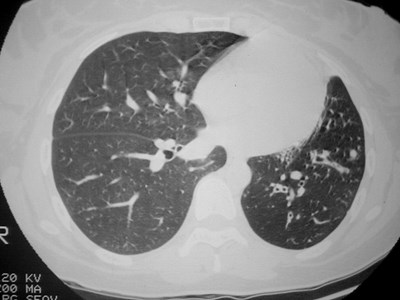
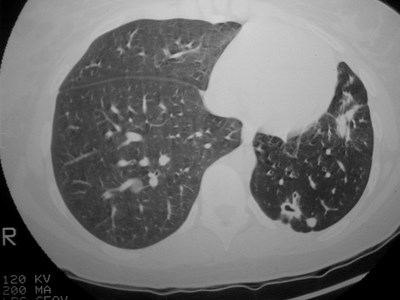
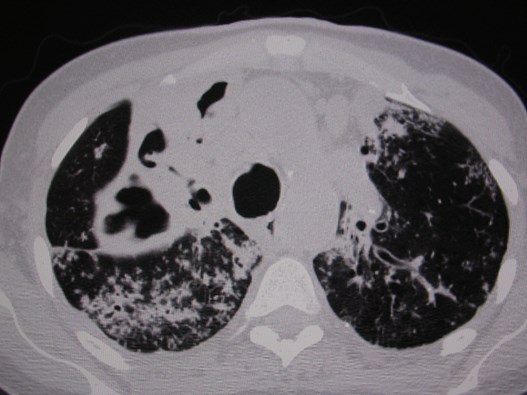
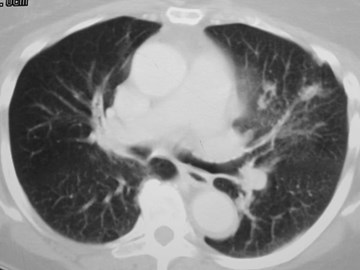
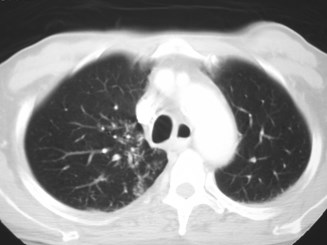
Postprimary (Reactivation) TBRadiology
•Heterogeneous opacities whichcan coalesce.
•Cavitary disease in 45%.
–Thick or thin walls
•Tuberculoma (up to 4 cm) mayhave Ca++
–Non-cavitary focus of disease.
–Usually sharply defined.
–May be more indolent disease.
•Satellite nodules helpful in dx.

























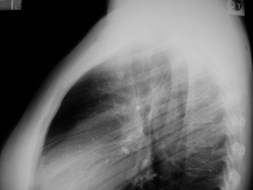
Additional views may help evaluate disease









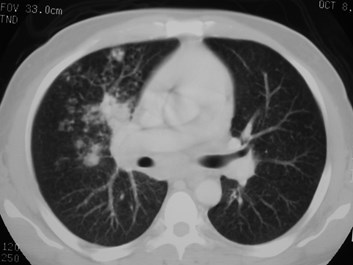
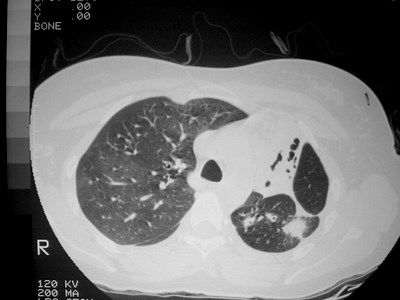
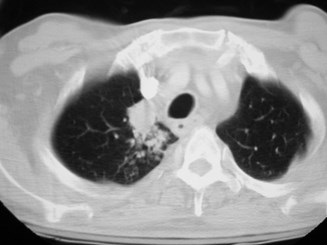
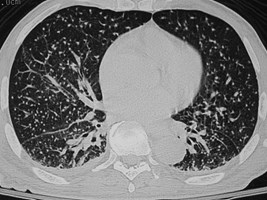
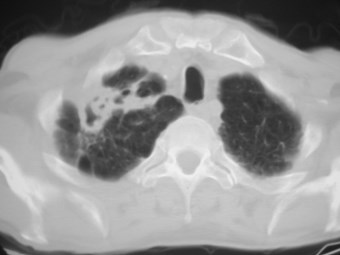
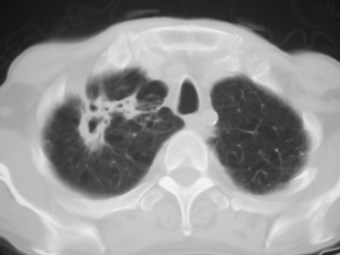
Postprimary (Reactivation) TBRadiology
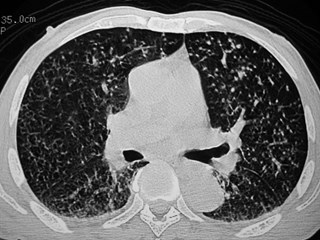
Endobronchial spread:
–5-10 mm nodules seen in up to20% on CXR
–Nodules seen in 95% on HRCT
–“Tree in bud”
•Clustered small centrilobular nodules
•“Jacks” and y-shaped nodules indicateimpacted bronchioles.



















Progressive TB
•Progressive destruction of lung tissue
–Necrosis and cicatrization
–Bronchiectasis
•Respiratory insufficiency as more lung is destroyed
•Hemoptysis
–Bronchiectasis
–Rasmussen’s aneurysm
•5 year mortality from untreated TB ~50%







































Multidrug resistant TB - India










TB can mimic cancer










































RUL wedge resection: caseating granulomas and AFB’s











Asymptomatic 42 yo






















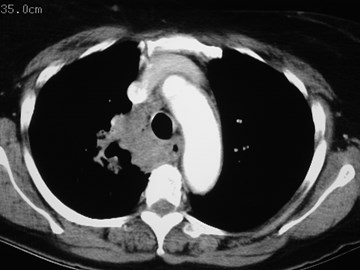
Postprimary (Reactivation) TB
•Lymphadenopathy unusual.
–5% of cases.
•Effusion uncommon.
–Up to 18% of cases.
–Air indicates bronchopleural fistula.
•Rupture of adjacent parenchymal focus.
–Often loculated.
–May form tuberculous empyema.
–Calcified fibrothorax (may have active organisms).



















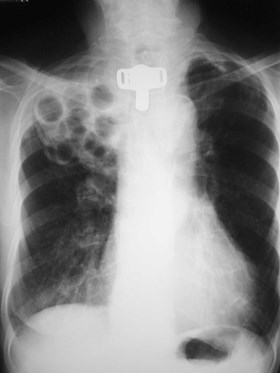
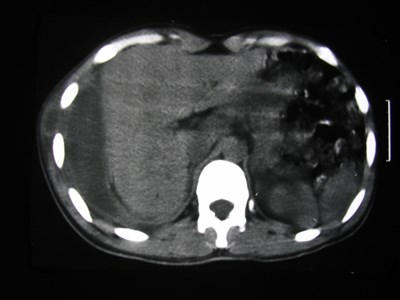
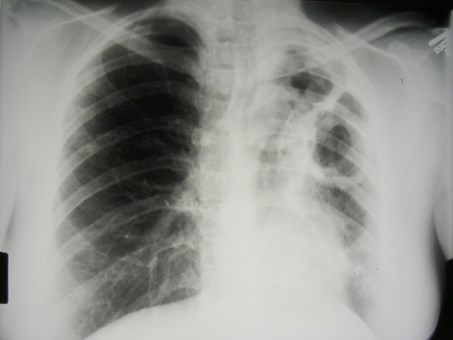
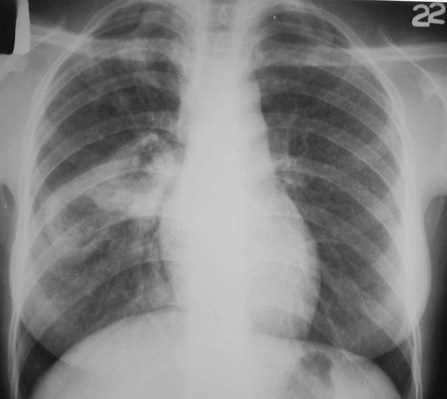
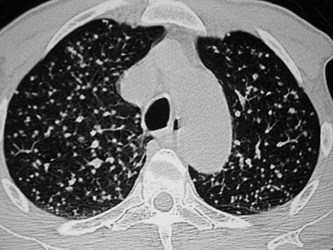
Miliary TB
•Lymphohematogenous spread toentire body.
•Occurs during primary infectionor reactivation.
•CXR abnormality takes 3-6 weeksto develop.
•25-40% with normal CXR.
•Diffuse distribution with slightbasilar predominance.
•1-4 mm nodules, uniform in size.

Millet seeds









Miliary TB
•Patient usually elderly, chronically ill
–HIV, ESRD, DM, EtOH
•Insidious onset
–Delayed diagnosis
–Nonspecific sx
•Cough, low grade fever, night sweats, wt loss
•Hepatospenomegaly
•PPD (-) in 25-50%
•Liver or bone marrow bx may establish dx




















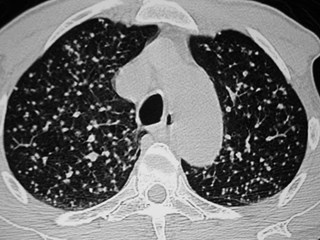











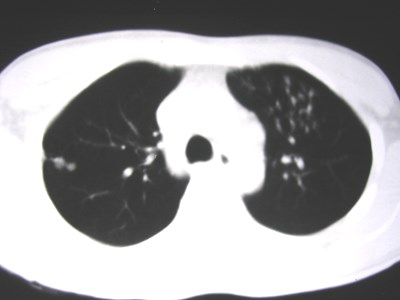
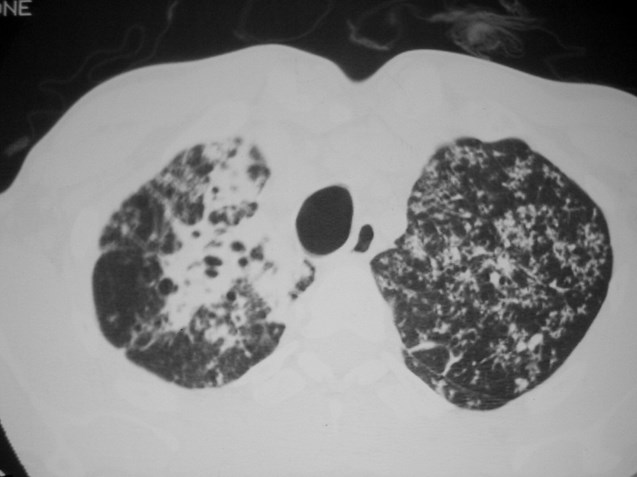
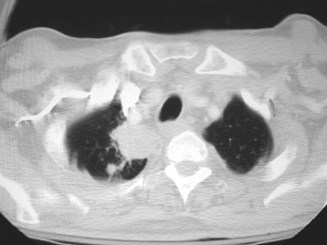
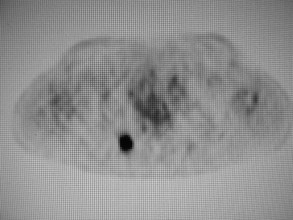
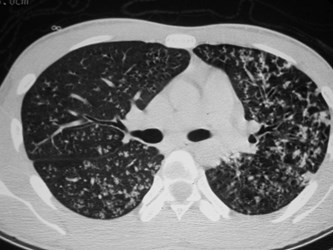
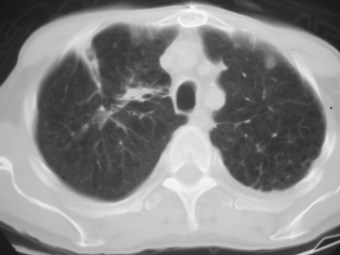
Miliary or Tree in Bud?










Miliary or Tree in Bud?
•Random
•Diffuse
•Only nodules
•Clusters
•Areas of sparing
•Jacks and Y’s









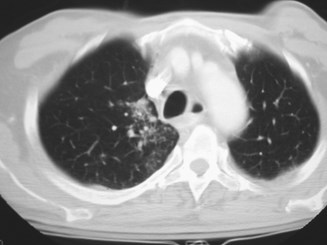
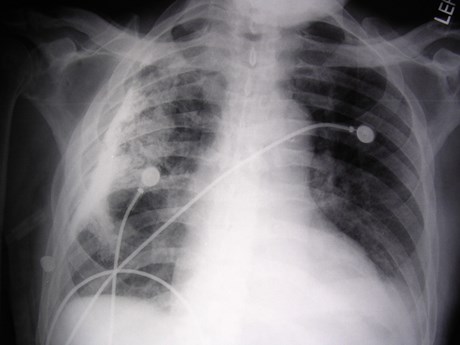
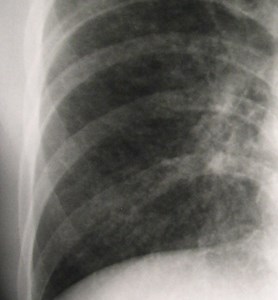
Active or Inactive Disease?
•Calcifications and fibrosis, even cavities are seenon CXR in both healed and active disease.
•CXR is usually not helpful unless findings arestable.
•“Tree in bud” nodules may be helpful.
•Diagnosis still requires isolation from sputum orbronchial washings.









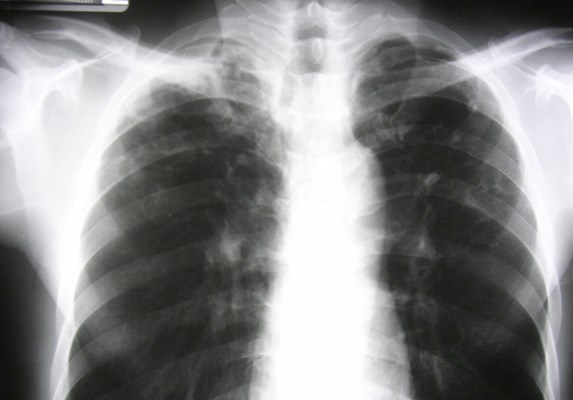


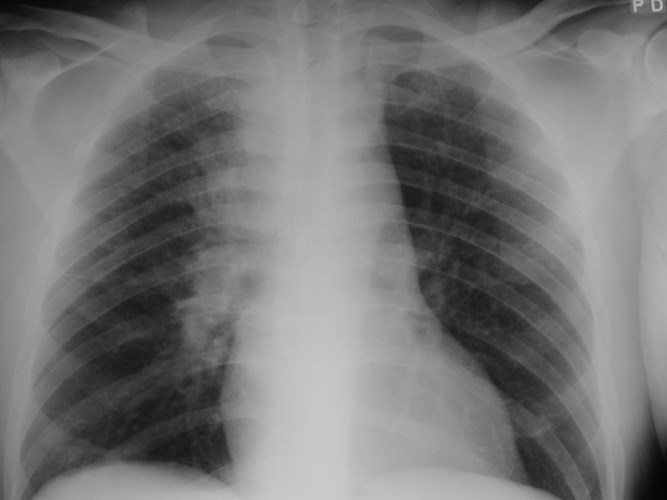
82 year old Korean man with cough









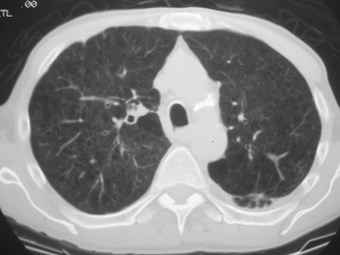
Cavity, bronchiectasis, fibrosis. Active disease?









Diagnosis
•Positive culture
–Standard cx 3-6 weeks
–Newer system 2-3 weeks
–DNA probe identifies TB inhours from culture specimen.
•Clinical and radiologicalevidence of active disease
•Acid fast organisms insputum or histologicspecimen









TreatmentLatent Disease
•+PPD, no signs of clinical disease.
•Decision to treat depends on:
–Age
–Size of reaction
–Recent contact?
–Immune status
•If normal CXR, 6-9 mo INH.
•If CXR shows old disease or immune compromised, 9 mo INH.
•Follow up CXR usually only if sx develop.
•<2% lifetime risk of active disease developing after Rx.









TreatmentActive Disease
•First line therapy
–INH, rifampin, ethambutol, pyrazinamide x 2 mo.
–then INH, RIF x 4 mo.
•Second line drugs
•cycloserine, ethionamide, streptomycin, amikacin,capreomycin, p-amino salicylic acid, levofloxacin
•Response: >80% cx-negative after 2 mo.
• risk of relapse: cavitary disease, (+) cx at 2 mo.
–Extend therapy to 9 mo.






















The End